TOBACCO USER STATUS AND CESSATION PROGRAM
Tobacco User Status
Employee Partners and spouses who are enrolling for the 1st time in the Medical Plan and who wish to receive contribution rate discounts for the Medical Plan. You must confirm/select your tobacco user or non-user status as well as the status of your spouse as the first step of the enrollment process on ESS. You must select a Tobacco Usage status even if you are not enrolling in the medical plan.
Tobacco Cessation Program
Invited is offering a FREE tobacco cessation program called Smokeless® to all Invited Employee Partners and their spouses who use tobacco products. In addition to the program kit, participants will receive coaching from certified lifestyle coaches. You must complete the Tobacco Cessation program within 90 days of your benefits effective date.
To enroll in the program and receive your free kit, please call 800.345.2476, press 1, hours of operation 8:00 - 5:30 est.
If you have benefits questions, send them to psbenefits@clubcorp.com
BENEFITS FORMS
| General 2022 Benefits Guide - English | Spanish Medical Declaration of Adult Dependent Prescription Drug Formulary Prime Mail FAQ Dental DHMO Highlights DPO Highlights Claim Form Vision Vision Plan Highlights - English Spanish Member Guide Claim Form |
Life Insurance Evidence of Insurability Beneficiary Resource Guide Dependent Care FSA DCFSA Claim Form Individual Investment Program (IIP) IIP Enrollment Guide IIP Plan Document Tobacco Cessation Program Tobacco Cessation Program Dependent Eligibility Verification Dependent Verification Information Dependent Verification Transmittal Form Employee Self Service (ESS) ESS Benefit Enrollment Guide |
If you have benefits questions, send them to psbenefits@clubcorp.com
BENEFITS CONTACTS
| Invited Benefits | www.Invited.com/benefits | psbenefits@clubcorp.com | 800.800.4615 (M-F, 8a-5p CT) | |
| Medical | United Healthcare | www.myuhc.com | 800.865.9386 |
|
| Telemedicine | 24/7 Virtual Visits | www.myuhc.com/virtualvisits | 855.615.8335 | |
| Prescription | RxBenefits | customercare@rxbenefits.com | 800.334.8134 |
|
| Dental | Delta Dental DPO Delta Dental DHMO |
www.deltadentalins.com | 800.521.2651 800.422.4234 |
Group #5813 Group #76217 |
| Vision | Superior Vision | www.superiorvision.com | 800.507.3800 | Group #34013 |
| Disability | Short Term Disability Long Term Disability |
www.metlife.com/mybenefits | 800.GET.MET8 | Group #119217 |
| Flexible Spending Account | TaxSaver Plan | www.taxserverplan.com | 800.328.4337 | Group: Invited |
| Employee Assistance Program (EAP) | LifeWorks | www.metlifeeap.lifeworks.com | 888.319.7819 | Username: metlifeeap Password: eap |
If you have benefits questions, send them to psbenefits@clubcorp.com or call Benefits Department at 800-800-4615.
BENEFITS FREQUENTLY ASKED QUESTIONS
Q: How do I get my username and password for Oracle HCM Employee Self Service (ESS)?
A: Contact the Invited Help Desk to secure your Oracle HCM ESS username and temporary password by calling 972-888-7777. The password is good for 24 hours only.
Q: Where do I go to sign up for Invited Employee Partner Benefits?
A: Log on to Oracle HCM ecwl.fs.us2.oraclecloud.com.
Q: Can I make any changes to my benefits after open enrollment or throughout the year?
A: Yes, you can make changes to your benefits after open enrollment and throughout the year IF you have a Qualifying Life Event (QLE) and you contact benefits within 31 days of the QLE.
A QLE is an experience that changes a person’s family or work status, like change in marital status or employment status.
Q: How can I view my current or future benefits?
A: See viewing instructions below:
- Contact the Invited Help Desk to secure your Oracle HCM ESS username and temporary password by calling 972-888-7777. The password is good for 24 hours only.
- Once you have your ESS username and password, log on to ecwl.fs.us2.oraclecloud.com.
- Select the orange Benefits icon.
- Select the View current and Future Benefits Icon.
- Your current coverage will appear
- To confirm coverage for 2020, change the Effective Date in the top left corner to 1/1/2020
Q: What is Telemedicine and what can it be used for?
A: Access to a licensed physician by phone 24 hours a day, 7-days for conditions like allergies, insect bites, fever, cold and flu, to name a few.
If you are enrolled in any medical plan or if you enroll in Plan D – Limited Medical, you will have access to Call-A-Doc physicians, who can diagnose you by phone and even send a prescription to your local pharmacy, quickly, easily, and conveniently. Just call 844-DOC-24HR (844-362-2447). A nurse will answer your call, take your medical history and arrange a call with a physician in your state within 3 hours.
Q: I have had a baby and I want to add them to my benefits. What do I do?
A: Within 31 days of your newborns birth, adoption foster placement, you can add them as you have experienced a change in family status supporting a Qualifying Life Event (QLE). Contact the Invited Benefits department within 31 days of the birth or placement with supporting documentation.
Q: How do I verify my dependent for Medical plan coverage?
A: You provide the required documents within 31 days of the coverage effective date. To get more information about the verification documents, please go to www.Invited.com/benefits and select Eligibility (EP & Dependents). If you do not verify your dependent within 31 days, their coverage will be cancelled with your coverage remaining in effect for the remainder of the year.
Q: Where do I send my Dependent Verification paperwork?
A: During Open Enrollment, it is sent to our verification vendor, MacGregor and Associates, and must be received on or before November 27, 2019.
Outside of Open Enrollment, please send your Dependent Verification information to psbenefits@clubcorp.com within 31 days of your effective date.
Q: What do I need to do if I think I might be going out on leave of absence?
A: You MUST contact Invited Benefits Department at 800-800-4615 or psbenefits@clubcorp.com before your leave of absence. The Invited Benefits Department will be able to help you and answer questions related to any leave of absence. Please reach out BEFORE you take any time away from work.
Q: How do I change or view my life insurance Beneficiary(ies)?
A: Contact the Invited Benefits Department if you want to add, change or update your beneficiary(ies). If you want to view your beneficiary(ies), follow the instructions below:
- Contact the Invited Help Desk to secure your Oracle HCM ESS username and temporary password by calling 972-888-7777. The password is good for 24 hours only.
- Once you have your ESS username and password, log on to ecwl.fs.us2.oraclecloud.com.
- elect the orange Benefits icon.
- Select the View current and Future Benefits Icon.
- Scroll down to Basic Life/AD&D on the Enrollment Summary page to view your beneficiary(ies) designation.
Q: How do I enroll in the Tobacco Cessation Program?
A: To enroll in the program and receive your free kit, please call 800.345.2476, press 1, hours of operation 8:00 - 5:30 (ET).
Q: How long do I have to submit my Tobacco Cessation program completion certificate?
A: You must complete the Tobacco Cessation program and send your completion certification to the Invited Benefits Department within 90 days of your benefits effective date.
Q: Do I need to submit anything if I elect Supplemental Life insurance for me and/or my family?
A: Maybe. If you are electing a supplemental life insurance in excess of 3x your annual salary or $380,000 (whichever is less), you will need to complete and submit to OneAmerica an Evidence of Insurability (EOI) based on the state in which you reside. You can find your EOI by clicking here.
Q: Can I elect Health Care Flexible Spending Account (HCFSA) and/or Dependent Care Flexible Spending Account (DCFSA) after Open Enrollment or make changes throughout the year?
A: Yes, you can make changes to your benefits after open enrollment and throughout the year IF you have a Qualifying Life Event (QLE) and you contact benefits within 31 days of the QLE.
A QLE is an experience that changes a person’s family or work status, like change in marital status or employment status.
Q: What is the difference between Health Care Flexible Spending Account (HCFSA) and Dependent Care Flexible Spending Account (DCFSA)?
A: The HCFSA is a tax-sheltered account that you fund to pay for predictable health care expenses (medical, dental, and vision) that are not covered or are only partially covered by your plans.
The DCFSA is a tax-sheltered account that you fund to pay for care-provider expenses related for children (such as a daycare provider, nanny, preschool, after school program, etc.) up to age 13 and for dependent adults who cannot care for themselves.
Q: Who are our benefit carriers?
A: See chart below:
| Contacts | Website | Telephone Number | |
| People Strategy Benefits Department | www.Invited.com/benefits | 800.800.4615 | |
| Invited Help Desk | 972.888.7777 | ||
| Medical | WebTPA | www.webtpa.com | 877.487.4300 |
| Telemedicine | Call-A-Doc | 844.362.2447 844.DOC-24HR |
|
| Prescription | NBFSA | 888.424.4186 | |
| Dental | Delta Dental | www.deltadentalins.com | DPO 800.521.2651 DHMO 800.422.4234 |
| Vision | Superior Vision | www.superiorvision.com | 800.507.3800 |
| Disability Insurance | OneAmerica | oneamerica.claims@customdisability.com | 855.517.6365 |
| Flexible Spending Account | TaxSaver Plan | www.taxsaverplan.com | 800.328.4337 |
| Individual Investment Plan (IIP) | Milliman Benefits | www.millimanbenefits.com | 866.767.1212 |
| Employee Assistance Program (EAP) | ComPysch | www.guidanceresources.com Web ID is ONEAMERICA3 |
855.387.9727 |
Q: How do I find network health care providers (hospitals, doctors, pharmacies)?
A: Go to WebTPA and click on XXXXX. This will open up the Aetna ASA network search.
Q: What happens if I go Out of Network?
A: If you go to a health care provider who is out of network, you have to pay 50% of the cost once you have satisfied the deductible. Additionally, if you have not pre-approved with WebTPA, the services may not be covered at all. To see if pre-approval is required, call WebTPA at XXX-XXX-XXXX.
Q: What does the Limited Medical Plan cover?
A: See Limited Medical plan below. For more information, call XXX-XXX-XXXX.
With the Limited Benefit option, you and your eligible dependents have access to:
- Prescription drug program administered by NBFSA
- Unlimited free telemedicine visits with a licensed physician, 24 hours a day, seven days a week
- Generic drugs for $0 - $25 (or actual cost, if less) and discounts of 30-85% off retail prices on brand-name drugs
- Dental and vision discounts
- Discounts shopping, dining and entertainment
- $10,000 of Accidental Death & Dismemberment (AD&D) insurance
Q: What is SurgeryPlus and where can I find more information?
A: SurgeryPlus is a highly effective and efficient network of best in-class doctors for specific non-emergent procedures, like back, knee or shoulder surgeries. If you are covered under Invited’s medical plan, you have access to the SurgeryPlus Surgeons of Excellence network. You can find more information by going to Invited.SurgeryPlus.com.
Q: What is the difference between the Delta Dental DPO and DHMO plan?
A: Both plans provide comprehensive dental coverage. However, there are two main differences. Number one, Delta Dental DPO allows you to go to any dentist and Delta Dental DHMO requires you select from a list of contracted DHMO dentists. To find a contract DeltaCare USA dentist, contact Delta Dental at www.deltadentalins.com (DeltaCare USA option) or call 1-800-422-4234. Number two, the cost for services is different between the two. For more information click here.
Q: Who is eligible for Short-Term Disability (STD) and Long-Term Disability (LTD)?
A: You are either eligible for STD or LTD, but not for both.
Long Term Disability (LTD) eligibility requires you be in one of the following positions to be eligible to participate in the LTD Plan:
- Home Office and Regional Staff,
- General Managers, or
- Salaried Department Heads who are primarily responsible for managing a department, such as (but not limited to): Athletic Director, Executive Chef, Food & Beverage Director, Golf Course Superintendent, Head Golf Professional, Head Tennis Professional, Membership Director, Member Relations Director, Operations Manager, Private Event Director or Service Director.
Short Term Disability (STD) eligible Employee Partners not eligible for the LTD Plan may participate in the STD Plan (except for Employee Partners working in clubs located in California, New Jersey or New York due to state-mandated disability plans already made available to you).
Q: How do and when can sign up for the Invited 401(k) plan?
A: Employee Partners become eligible for the IIP if the 1) are full-time or part-time regular, 2) age 21 or older and 3) have completed six months of continuous service with Invited. You can sign up by going to www.millimanbenefits.com. The first time you log on to the website, your will be asked to provide your Social Security number and password. Your password will be your month and year of birth (MMYY).
COVID VACCINATION INCENTIVE
Covid Vaccination Incentive
During 2022 Open Enrollment, you either made a 2022 medical plan election and/or your COVID-19 vaccination status indicated you and your spouse (if applicable) are fully vaccinated and therefore eligible to receive the $50 COVID Wellness Incentive. It is now time to provide proof of vaccination.
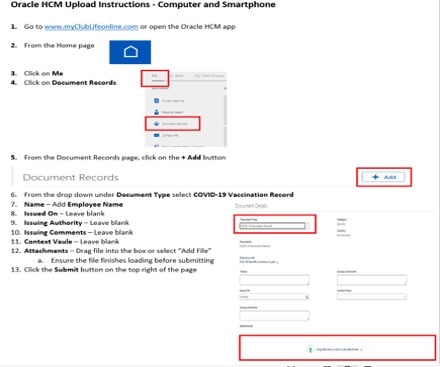
You will be uploading proof of the COVID-19 vaccination into Oracle HCM via the computer or your smartphone.
The instructions for providing proof of the vaccination by computer and smartphone is below in English. Attached are the instructions in both English and Spanish. Instructions for downloading the Oracle HCM app is also in the attached document.
If you already uploaded your proof of vaccination or emailed your proof of vaccination to the Benefits Department, we are currently in the process of reviewing and validating. Please know that if there is any missing information, we will be reaching out.